An anonymous HVCS employee’s remembrance in observance of STI Awareness Month
During my junior year of college, I worked off campus at a big-box retail store with a closeted guy named Orin*. We occasionally but infrequently hooked up, usually at his apartment. One night my roommate was away, and I invited Orin back to my dorm room for a hook-up. I usually had a stash of condoms, but I was out that night—so we both shrugged and threw caution to the wind. As we had had sex before, I thought, “I didn’t catch anything last time, and he looks healthy.” Never mind that “last time” was a few months ago, and it was almost pitch-black in my room.
Within a few days, urinating felt like a shower of needles. It was a sharp, tingly pain that made me dread the next bathroom break. I powered on through classes and work, determined to ignore the slivers of agony and refusing to admit that I’d made a mistake. I also avoided Orin, though I wanted to demand, “What did you do to me? Aren’t you feeling this pain too?”
Feeling Worse
I traveled to Virginia to spend Thanksgiving with my family. The burning in my urethra started to linger long after urinating, and I struggled to stay in “celebratory holiday mode” as the weekend dragged on. We had lunch at a fish n chips restaurant that was touted as a favorite among locals for its fresh catches. Within hours, I hovered over the toilet bowl, returning the meal, and a lot of other stuff, to the sea. I spent the rest of the holiday in my brother’s bed, shivering, in growing groin agony, popping Tylenol to lower my fever in between trips to the bathroom to puke. My sister-in-law endured the same symptoms, camped out in a spare bedroom. Mom’s verdict: food poisoning. For me, it was all coming out the top—and nothing, absolutely nothing, was coming out the bottom.
By Sunday when I returned to campus, my fever had abated but what I strongly suspected to be a sexually transmitted infection continued with a fury. I imagined my bladder swollen and red, angered by some tiny spirochete armed with a sword of ice. My intestines felt hard to the touch, and I had no interest in food of any kind. (Younger me also was blind to basic over-the-counter constipation remedies, for some reason.) My birthday falls soon after Thanksgiving, and I turned down all invitations to celebrate it at the local nightclub.
Later that week during my evening shift, I finally felt something happening in my nether regions. Warm liquid blossomed in my underwear, and I dashed to the restroom. It turned out to be a small amount, but it was red: I had bled and it had soaked through onto my jeans. Completely humiliated, I tied an apron around me, backwards, and fought with my boss to leave early. When he objected strongly, I told him the truth: I had a blood stain on my pants—“Don’t make me show you.” He let me leave.
Seeking Medical Care At Last
Finally, I was ready to go to the Student Health office. The regular doctor, whom I’d been to a few times over the years, was out, and a substitute provider was filling in. Now gripped with double the embarrassment of having to admit my mistake to a stranger, I told my story. “Well, sounds like an STD,” she said. “I’ll have to do a culture to be sure.” Obtaining a culture (back then)** involved many men’s worst nightmare: a swab up the urethra for a scraping. I endured this humiliation, zipped up, and went back to my dorm to wait for the test results.

The sub doctor called the next morning, and in essence she said: “You tested negative. Whatever you’re feeling is probably from the food poisoning and should go away soon.” End of call. I soldiered on through the week, steeled against the pain and discomfort. My bowels felt impacted—wasn’t food poisoning supposed to clear everything out?
On Monday morning, I got a call from the usual campus doctor. “I reviewed notes on the cases that came in while I was out, and yours stood out. Can you come over right now?” When I sat on the exam table, she said, “I think my sub was wrong. I think you do have an STD. I don’t know what she did wrong with the culture, but all your symptoms point to an STD. The burning when you pee, the constipation. You have a case of anal gonorrhea. Here’s a prescription for azithromycin.”
Within a day of taking the antibiotic, the burning sensation faded. The constipation took longer to resolve, but it did go away eventually. A friend with a keen eye spotted the medicine bottle on my dresser and asked about it, and I finally confessed: I had unprotected sex. He let loose a torrent of disappointment, admonishment, and concern. “You know better than that. Of all people, you? For a one night stand?” I explained that it wasn’t a one-nighter per se, which didn’t help my case. “I hope it’s a never again,” he said. “Did the doctor order an HIV test? No? Well, you need to get one ASAP.”
Confrontation
A few nights later, I wound up closing the store with Orin, and I finally worked up the nerve to say, “You gave me gonorrhea.” He wrinkled his nose and said, “It wasn’t from me. I feel fine.” Which makes perfect sense when you learn that many men with STDs are asymptomatic. I pushed back, stating that he had been my only sexual partner in the past month. He kept denying it. “Get tested,” I advised.
After two weeks of suffering, mixed with a case of food poisoning, a wrong medical diagnosis, an excruciating outing to my boss, and a missed birthday, I resolved to use condoms for every sexual encounter. I took an entire class on AIDS issues to understand better the science behind transmission and risk. That class led me to volunteering for HVCS. After I graduated, that volunteer work turned into a paid job.
All the literature and articles say, “it only takes one condomless encounter,” and while mine wasn’t technically “just one” with the same guy, the risk was certainly there. The HIV test came back negative, and from that point on, for at least a decade, I sero-sortied: only sleeping with men who were HIV-negative. There wasn’t, and still isn’t, a realistic way to sero-sort STD status, since it’s so hard to know if, and when, you have an STD.
Lessons Learned
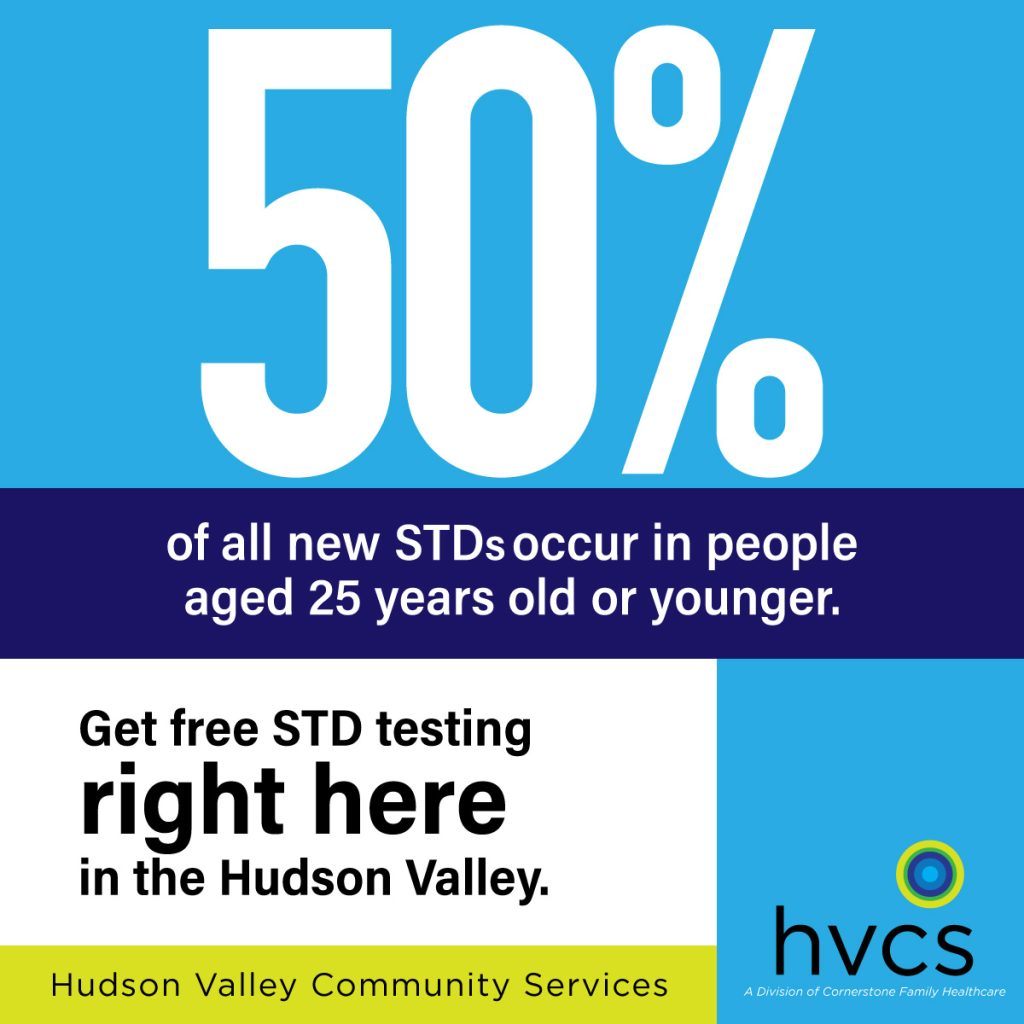
Looking back now, I wish I could say I “slipped up” on safer sex for burning passion, or drunken abandon, or some other (ultimately meaningless) excuse, but the truth was, changing the plan in favor of safer, non-penetrative acts was simply inconvenient. I didn’t have a great reason, other than laziness. The sheer stupidity of that (I’m allowed to call my actions stupid, aren’t I?) gave me insight into how others cope with the specter of HIV and other STDs. There are so many possible reasons for forgoing a condom: it’s very difficult for disease prevention programs, like those at HVCS, to give clients a road map to navigate all of those scenarios. With STIs (the more modern term for STDs) on the rise, empowering clients to be self-advocates for their sexual health is likely the best defense. Arm up with the facts—and take this post as a cautionary tale I hope you never have to experience for yourself.
*Name changed to protect the closeted.
** Today’s STI tests use a blood or urine sample.